Psoriasis
sr · ai · uh · suhsPsoriasis is a lifelong autoimmune disease in which skin cells build up and create rough, scaly patches. It’s not contagious, but it can cause psychological distress. The good news is that it can be managed over time.
Also Called
Plaque psoriasis
Frequently Found On
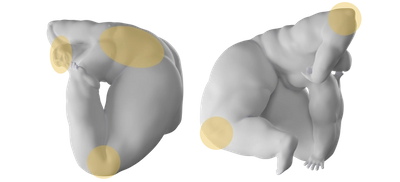
Elbows, knees, scalp, trunk
What is psoriasis?
Psoriasis is a tough one. It looks scaly and rough, red and menacing, and many people think it’s contagious. It’s not. But the look of those scaly patches, which are just an excess layer of skin cells, can cause serious emotional distress in people who have it. Which is a lot of people. Psoriasis is an autoimmune skin disease that affects over eight million people a year; it’s as common as eczema, and like eczema, there is no “cure.” So treating psoriasis is mostly about learning how to manage it over time with lifestyle and dietary changes, while targeted light therapy may help eliminate some patches.
A common misconception with psoriasis is that it’s related to dry skin, but it’s not. If your body is going to develop psoriasis, it has nothing to do with the dry winter weather. Therefore the treatment is slightly more complex than throwing on a few extra-thick lotions. Here’s what you need to know.
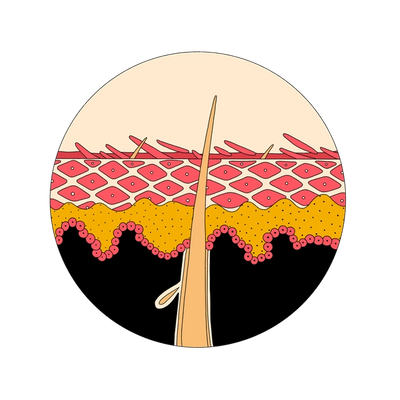
In an average human body, skin cells grow deep in the skin’s layers and then rise to the surface, eventually flaking off. A skin cell’s typical life cycle is about a month.
Psoriasis is an autoimmune disease that causes skin cells on the body to build up rapidly. This production process might only take a week or a few days, meaning that the skin cells have no time to fall off on their own. This leads to a thick, scaly-looking layer of skin cells that can become infected. More than eight million people in the United States are affected each year, so it’s more prevalent than it may seem.
Most psoriasis sufferers have plaque psoriasis, which includes large patches of red, scaly skin on isolated areas of the body. However, there are many other kinds of psoriasis that all have similar symptoms.
Dr. Lily Talakoub, a board-certified dermatologist at McLean Dermatology in McLean, Virginia, always tells psoriasis patients: “I cannot change the genes that you have, but I could really help you control the symptoms of it.”
With psoriasis, one size doesn’t fit all. Symptoms differ from person to person, and the severity can vary.
The most commonly affected areas are lower back, knees, elbows, and legs. However, flare-ups can also affect the feet, palms, scalp, and face. Many flare-ups occur cyclically, meaning that the symptoms will appear for a few weeks before subsiding for a time.
Typical signs of psoriasis might include:
- Red patches of skin covered in thick scales.
- Dry skin that may bleed, itch, or burn.
- Spotty, scaling patches.
- Swollen and stiff joints.
- Thickened or ridged fingernails or toenails.
Some people might have just a few dandruff-like spots on their scalp, while others might suffer from rashes that coat the entire body, though that’s very rare, and known as erythrodermic psoriasis.1
What causes psoriasis?
Since psoriasis is a condition that affects the immune system, researchers believe that psoriasis is a result of the body attacking itself.2 Specifically in psoriasis, certain white blood cells mistakenly attack skin cells, causing overgrowth.
Dr. Lily Talakoub points out that psoriasis is often genetic, so having immediate family members with psoriasis can increase your likelihood of developing it. One of the first questions psoriasis patients ask her are, “Did I do anything to do this to myself?” And the answer is, nope. Sometimes the body throws us for a loop. Psoriasis is one of those loops.
There are certain triggers that can cause a psoriasis flare-up more quickly than others. Eating inflammatory foods like dairy and sugar can cause inflammation in the skin, which can show up as red, scaly psoriasis.
But stress is one of the most common triggers for psoriasis. This is because stress can weaken the body’s immune system, making it more susceptible to all kinds of attacks, from the flu to skin conditions like psoriasis and eczema. And then psoriasis itself can cause stress, so it might feel like a vicious cycle. Learning how to manage that stress might take some time and require the help of a therapist or counselor, but that’s a huge component to the lifelong treatment of psoriasis (and supporting your mental health is always a good thing).
Psoriasis and Arthritis
Psoriatic arthritis—joint pain, swelling, stiffness–is a form of arthritis that may affect some people with a history of psoriasis.
“Again, it’s about inflammation,” says Dr. Talakoub. “The inflammation that circulates around your skin because of psoriasis also circulates around the joints, and causes inflammation of the joints, and that’s what causes arthritis.”
Psoriasis is the single greatest risk factor for developing psoriatic arthritis. Psoriasis on the nails is usually a sign that psoriatic arthritis might occur in the body at some point. Regular visits to your dermatologist and primary care doctor should closely monitor how that develops, and how to treat it.
How do you treat psoriasis?
Psoriasis has no cure; it will always exist in the body in some form among those who have it. However, treatments that aim towards reducing inflammation, slowing the growth of those skin cells, and removing plaque are all effective ways to manage psoriasis over a lifetime.
Topical Treatments
Treatment depends on how much of the body is affected by psoriasis patches. “If it’s less than 10%,” says Dr. Talakoub, “I usually start with a topical steroid cream and dietary modifications.”
Topical steroid creams, available over-the-counter at any drugstore, are applied directly to the skin and can reduce redness, itchiness, and inflammation associated with psoriasis. Topical steroids include corticosteroids and retinoids and come in a range of strengths, including prescription strength, so talk to your doctor before buying one.
Other topical options might be soaps with salicylic acid and coal tar, which clear away dead skin cells and can help minimize psoriasis patches. Or anthralin, a medicated cream that slows the body’s production of skin cells in that area. Synthetic vitamin D3 and vitamin A can also be applied as anti-inflammatories on the skin.
As with many skin conditions, it might take weeks to see results, so treating psoriasis can be slow-going, and there might be some trial-and-error before you fine-tune the treatment that works best for you.
Scalp Psoriasis Treatments
Scalp psoriasis, often confused with dandruff (which is caused by a fungus), affects around half of people experiencing psoriasis, and more often on skin of color. It usually appears around the hairline and neck as a thickened, raised patch of rough skin. It can be treated with shampoos medicated with salicylic acid, which helps clear away the excess skin, and coal tar, which helps slow skin cell production. These medicated shampoos are available over-the-counter and in stronger prescription varieties. Other treatment options exist for scalp psoriasis, like light therapy and biologics (immunosuppressive drugs), but a dermatologist will point you in the right direction for your skin.
Light Therapy
Also known as phototherapy, light therapy is becoming a popular treatment for severe psoriasis. Dr. Lily Talakoub, a board-certified dermatologist at McLean Dermatology in McLean, Virginia, notes that she turns to light therapy in patients with psoriasis covering around 50 percent of their body. Light therapy utilizes UVB light, which is also present in sunlight, to target specific regions of the skin. “The production of Vitamin D is protective in the skin,” says Dr. Talakoub. “It's anti-inflammatory”—meaning it can slow the growth of skin cells and clear psoriasis lesions.
Through artificial ultraviolet rays, the skin is exposed for a set length of time on a regular schedule. Unlike real sunlight, these fake rays are concentrated and controlled to be effective in a much shorter time than it would take to reap that sunlight’s Vitamin D benefits at the beach, without the skin cancer risk. The key to phototherapy’s success is consistency, so it’s important that the treatment is administered regularly.
There are home phototherapy units available too, but all forms of phototherapy require a doctor’s prescription.
Medication
If a patient has psoriasis covering 10 to 50 percent of their skin, Dr. Talakoub usually prescribes an oral medication, such as an oral retinoid that will help slow down the speed your skin cells are growing.
At around 50 percent—a pretty severe case—she’ll prescribe biologics, which are injectable drugs that moderate the immune system. “Remember how we were saying that the immune system is overactive in psoriasis? These medications downregulate the immune system so the immune system doesn’t overproduce the skin cells causing psoriasis,” she says. “So, it shuts down the immune system in a way, which can be great for people who have lots of lesions. It can clear them 100 percent, but it can also make you susceptible [to other illnesses] because your immune system is actually shut down a little bit.”
Because of this, doctors usually only prescribe these medications for short periods of time.
How do you prevent psoriasis?
You can’t completely prevent skin from developing psoriasis, but you can work to prevent flare-ups. Lifestyle changes, especially in diet, are the key to managing short or long-term psoriasis.
Managing Diet
“There’s a huge dietary component with psoriasis,” says Dr. Lily Talakoub. Taking Vitamin D, which is anti-inflammatory, can protect the skin from the inside (as well as from the outside, if you do phototherapy). It keeps the skin from overdeveloping cells that turn into psoriasis patches. Avoiding foods that are inflammatory in the body, like dairy, gluten, sugars, and processed foods can help prevent psoriasis by removing those inflammatory triggers.
“It helps, but it’s not curative,” reminds Dr. Talakoub. “But definitely, for people who are overweight, or eating a lot of sugar and dairy and other highly inflammatory foods, it'll make the psoriasis flare.”
Eating anti-inflammatory foods that are rich in omega-3 fatty acids, such as fish, berries, green leafy vegetables, seeds and nuts, can therefore help reduce psoriasis flare-ups.
(Data on patients with psoriasis shows that people with psoriasis have a higher risk of stroke, heart disease, diabetes, and obesity than those who don’t.)3
“It's hard to get somebody to change their diet,” admits Dr. Talakoub. “It’s easier to give them medication. And that’s the problem. We need to really focus on changing our nutrition to help prevent disease, rather than give drugs to help treat disease.”
So if you’re—understandably!—overwhelmed with the idea of changing your diet to manage psoriasis, talk to a registered dietitian about it. They can help set up an eating plan that reflects your tastes and habits, rather than jump into a complete overhaul that you can’t sustain.
Mental Healthcare
Psoriasis can be socially stressful, especially if the patches are in visible areas, like the elbows. Imagine having to constantly tell people you meet that “no, it’s not contagious, it’s an autoimmune disorder, it flares up when I eat ice cream...” when they look at you with concern or even fear.
“When somebody has red stuff all over their skin, it's obviously external,” says Dr. Talakoub. “If you have these red spots all over your arteries, nobody could tell. But people are embarrassed by [psoriasis]. It does affect self-esteem. It is stigmatizing. People worry that it’s contagious when they see it, and it’s not.”
Studies have found psoriasis linked to sleep and sexual problems, self-esteem, substance abuse, eating disorders, and other mental illnesses.4 So while dermatologists can help patients manage the skincare aspect of psoriasis, it’s also crucial to address the emotional toll it may be taking, and seek psychological support when needed. Getting more sleep, meditating, taking calming baths or long walks, can help decrease stress and keep your psoriasis flares under control—or maybe a bath won’t be enough. Just because your body has created this skin condition doesn’t mean you have to face it alone.
Citations
1Erythrodermic psoriasis: pathophysiology and current treatment perspectives by Rasnik K Singh et al. Psoriasis (Auckl).
2Psoriasis Pathogenesis and Treatment by Adriana Rendon and Knut Schäkel. Int J Mol Sci.
3Psoriasis and Cardiovascular Diseases: A Literature Review to Determine the Causal Relationship by Shanu Jindal and Nitin Jindal. Cureus.
4Psoriasis and Associated Psychiatric Disorders by Bárbara Isabel Roque Cunha Ferreira, MD et al. J Clin Aesthet Dermatol.
Additional References:
Diagnosis and management of psoriasis by Whan B. Kim, MD et al.
Get Updates
There’s more to come.
Sign up to receive periodical updates on Mass Index, and to be the first to know when Soft Services launches new products. (If we don’t have any updates, we won’t email you.)




















