Fungal Infections
fuhng · gl -uhn · fek · shnzThere’s a microbiome of fungus on the skin, and sometimes an excess of fungus can cause an itchy, annoying infection. They’re as common as they are treatable, which is very.
Also Called
Athere's foot, jock itch, tinea veriscolor, fungal acne (pityrosporum folliculitis)
Frequently Found On
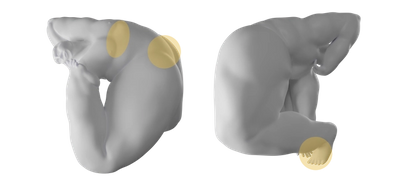
Areas of the skin that are dark, damp, and warm, such as the feet, in between toes, folds of skin, the groin, and underneath the breasts
What are fungal infections?
These things are normal, normal. [Fungal infections] happen to nearly everybody at some point in their life.
—says Dr. Caren Campbell, a board-certified dermatologist in San Francisco, CA.
Sometimes, a fungal infection can feel like it came out of nowhere. And it might have. The skin is constantly changing, and it’s made up of thousands of microorganisms that try to live together in harmony, but sometimes that balance gets out of whack. Infections happen. They’re usually itchy.
But fungal infections can be tricky to identify because of how similar they appear to many other skin conditions, like eczema. A dermatologist is trained to identify them. So if you’re unsure if a rash is an infection, an allergic reaction, or a witch’s curse, visit a doctor for a proper diagnosis.
Fungal infections are sometimes referred to as mycoses.1
There are millions of species of fungi all over the planet. But slicing mushrooms for dinner won’t lead to a fungal skin infection. The fungus responsible for most fungal skin infections exists naturally on the human skin at all times. “The malassezia yeast lives on everybody’s skin,” says Dr. Caren Campbell. “And it likes to overgrow in oil-rich environments. That includes sides of the nose, in between the eyebrows, on the scalp, behind the ears, and on the central chest of men.” Those are some, but not all, possible areas of fungal infection.
Yeast is a fungus that helps to foster skin health. To put it briefly—because the skin microbiome is a complex topic that’s still being studied—the amount of yeast on the skin is balanced out with “good” bacteria; they co-exist so that neither one becomes too abundant.2
But when this equilibrium is thrown off-balance, it can lead to an infection. Too much bacteria and oil can lead to acne. But too much fungi could lead to a variety of different infections in multiple locations on the body—usually places that get dark and moist, though, because that’s where fungi thrive. Common types of fungal infections include dandruff (seborrheic dermatitis), fungal acne (pityrosporum folliculitis), tinea versicolor, jock itch (tinea cruris), ringworm, yeast infections, and athlete's foot (tinea pedis).

The important thing to remember about fungal infections is that they’re rarely life-threatening and they’re often easily treated with over-the-counter antifungal creams.
Fungal Infections vs. Bacterial Infections
Bacteria and fungi live on the human body to provide a number of benefits necessary for healthy living, even though you can’t see them. But fungi are more complex organisms than bacteria.
Fungi are eukaryotes, which means they’re composed of cells that have a nucleus. Bacteria are prokaryotes, so they’re single-celled and have no nucleus. What this means for humans is that bacteria are much more adaptive and sly, and they’ll mutate much faster than fungi. (Don’t worry, there won’t be a pop quiz.)
But this is why fungal infections are often easier to treat, because the organism is slower to mutate and change, which means treatments can act quickly.
For example, the most common bacterial infection on the skin is a Staph infection, named after staphylococcus bacteria, the natural bacteria that lives on the skin. Staph infections can enter the bloodstream and cause a host of other, sometimes very serious, problems. Treating them might require prescription antibiotics.
On the other hand, fungal infections might present as an itchy patch that can be treated with a topical cream and dealt with in a few weeks. Of course, this is very, very generally speaking. For any skin condition that’s outside of the norm, have a doctor check it out to get a proper diagnosis. Neither should be left untreated.
Types of Fungal Infections
There are too many types of fungal infections to even count. These common fungal infections only begin to scratch the surface.
Athlete’s Foot
One of the most common fungal infections is athlete’s foot, or tinea pedis. As you might guess, it often occurs in athletes or people who find themselves barefoot in a shared space like a locker room, public showers, or pool deck. But it can also affect people who have sweaty or still-damp feet, who then wear shoes all day. Fungus grows in dark, damp spaces, so you can see where this is going. Athlete’s foot can be contagious, spreading on the locker room floor, but it can also show up of its own accord if the conditions are just right.
Athlete’s foot might start with an itch and look like a red rash. But if it grows, it might cause peeling, blisters, and scaliness on the feet, typically between the toes. Sometimes it might cover the entire sole, and other times it might just be a few small patches. Over-the-counter antifungal creams and sprays usually take care of it; while drying powders, and making sure to wash and really dry the feet before putting shoes and socks on, can help prevent it. (Skip ahead to see how you treat athlete's foot.)
Jock Itch
Jock itch, like athlete’s foot, isn’t named with subtlety. It’s medically known as tinea cruris, and yes, it primarily affects athletes, but that doesn’t mean only people who wear jerseys and drink sponsored Gatorade can get it. Anyone who’s sweating in the groin region, man or woman, can experience jock itch. It’s an itchy, red rash in the folds of skin in the groin area and inner thighs. It might peel and flake.
As with many fungal infections, it’s more common during warm and humid summer months, though it can happen at any time of year. Jock itch is usually caused by not changing workout clothes or failing to properly clean and dry the groin area during and after showering. In some cases, it might be caused by a contagious case of athlete’s foot. It could also be caused by sharing contaminated towels or clothing. But also like athlete’s foot, it can be easily treated with hydrocortisone and/or antifungal treatments, often labeled specifically for jock itch. More severe cases might require a prescription ointment or oral antifungal. (Skip ahead to see how you treat jock itch.)
Tinea Versicolor
Tinea versicolor is a common fungal infection that affects the normal pigmentation of the skin, hence the word “versicolor.” It results in small to large patches of discolored skin that might be lighter or darker than the surrounding area, though in most cases, the discoloration is lighter.
“Tinea versicolor is a common condition in the summer,” says Dr. Caren Campbell. “Yeast [on the skin] produces what’s called azelaic acid—which is used in a lot of cosmetics for helping with hyperpigmentation—and that azelaic acid interferes with pigment production, so it causes these little white patches on the skin.” Because the skin isn’t internally creating the melanin that gives skin its color, white patches of tinea versicolor won’t tan.
Oily skin and humid weather are among the greatest causes of tinea versicolor. It can be treated the same way as other fungal infections, with topical antifungal creams, dandruff shampoo used as a body wash, and prescription medication for more severe cases. (Read more on how you treat tinea versicolor.)
Fungal Acne
Fungal acne is one of the trickiest fungal infections to identify because of how similar it appears to acne, hence the nickname. But fungal acne isn’t a medical term, and it’s misleading because fungal acne isn’t related to acne at all—it’s a fungal infection caused by an overgrowth of yeast.
[Fungal acne is] not a thing. It doesn’t exist. It’s not a medical term.
—says explains Dr. Caren Campbell, a board-certified dermatologist in San Francisco, CA.
In most cases, she notes, people use “fungal acne” to refer to pityrosporum folliculitis, the medical term that indicates a fungal infection that’s clogging the hair follicles. But the nickname, thanks to social media, has stuck.
Pityrosporum folliculitis—fungal acne—causes small, uniform pimples that look like whiteheads in certain areas of the body, primarily the chest, back, or arms, and in rare cases, the face. Like other fungal infections, it can be red, inflamed, and itchy. It’s typically treated with sulfur washes, or ketoconazole dandruff shampoo used as a body wash.
Products used to treat acne (acne vulgaris) don’t work on fungal acne, because the cause of fungal acne is completely different. Pityrosporum folliculitis, fungal acne, is caused by an overgrowth of yeast, which can happen when there’s trapped moisture on the skin, say from sweaty workout clothes—or any sweaty/damp clothes—left on too long. It can also happen as a side effect of certain medications, or totally randomly, due to one’s unique body chemistry.
Fungal acne has a “monomorphic” distribution.
—notes Dr. Campbell, which means every tiny pimple-like bump is around the same size.
Acne vulgaris usually shows up with pimples of different sizes, scattered here and there, and they typically don’t itch. A dermatologist will be able to immediately spot the difference. (Read more on how you treat fungal acne.)
Intertrigo
Intertrigo is a general term for red, inflamed skin in areas where there are skin folds. But it can have a fungal component, notes Dr. Caren Campbell. “It’s like jock itch,” she explains. “[It can occur] in women who have larger breasts. You get these shiny, pink patches on the skin under the breasts, or in the groin fold of men.” The yeast overgrows in warm, moist areas, which is why it’s commonly found underneath the breasts, in the armpits, and groin.
It can be treated with antifungal topical creams, or oral medication, and prevented with over-the-counter drying powders, like Zeosorb, that help sweat from accumulating on those areas of the skin.
Dandruff (seborrheic dermatitis)
Seborrheic dermatitis usually refers to dandruff on the scalp, but it can also present as flaky patches in between the eyebrows, behind the ears, and elsewhere on the body. “A large percentage of the population has seborrheic dermatitis,” notes Dr. Caren Campbell. But despite how common it is—one study mentions half the population experiences it—doctors aren’t totally certain what causes it, though they believe there’s a fungal component.3 Fungus usually grows in damp, dark environments, but it can also grow in oily areas of the skin, like the scalp.
The typical treatment is an antifungal dandruff shampoo. But “it's a spectrum, just like anything in life,” Dr. Campbell says. Mild cases can be treated with over-the-counter shampoos like Selsun Blue, she notes, while “other patients, who might have oilier skin or for whatever reason, their genetic makeup predisposes them to more significant overgrowth of that yeast, might need prescription-strength antifungal shampoos, creams, pills, or topical agents.”
Onychomycosis
Although it sounds serious and is definitely hard to spell, onychomycosis is just a fungal nail infection. It’s more common on the toenails than fingernails, because toes are a better breeding ground for fungus (especially when hidden in socks), but it can occur in both areas.
Onychomycosis is usually identified by discolored nails that appear either yellow or brown. It can also cause the nails to thicken, or become brittle or painful to the touch.4 It can be caused from fungus overgrowth, athlete’s foot, unsterilized nail clippers, and the infection can become much worse in patients with diabetes, or who have blood circulation issues.
Because of the sensitive nature of this infection, prescriptions are usually necessary to treat it rather than over-the-counter antifungal creams.
What causes a fungal infection?
It might seem like a fungal infection is an invasion. Who invited this fungus to the party? But the truth is, there’s always fungus on the skin, you just can’t see it, no matter how close you get to the mirror. Fungus is one of many microorganisms that keep the skin healthy and protected, but like fungus in the wild—you know, mushrooms—it can grow. Where there are warm, dark, and damp areas of the skin, fungus can make itself at home. An overgrowth of fungi is what usually causes a fungal infection.
In rarer instances, you can get a fungal infection from contact with certain plants and animals. “There’s microsporum canis,”—a fungal infection from dogs—says Dr. Caren Campbell, a board-certified dermatologist in San Francisco, CA. “There’s even a fungus that you get from tending to roses.” But for the most part, fungal infections are caused by the category of fungus that naturally occurs on our skin, known as malassezia.
Damp and Dark Environments
Fungi breed in areas that are warm, dark, and moist. On the skin, that might be in between the toes, in folds of skin, in the groin area, armpits, or underneath breasts. Fungi also breed in oil-rich areas, like the scalp. When we create these environments on the skin, just by wearing clothing, sock, and shoes, we begin to create the conditions for fungi to grow. Sitting around in damp clothing can create the perfect storm.
That said, “some people are more prone to yeast than others just based on their intrinsic body chemistry,” notes Dr. Joyce Imahiyerobo-Ip, a board-certified dermatologist and the CEO of Vibrant Dermatology in Greater Boston, MA. Two people on the same track team might experience entirely different skin reactions after sitting around in their sweaty running gear.
To prevent a possible fungal infection, it’s important to change clothes after sweating excessively. Ideally to shower, dry off well, and then change clothes.
Communal Surfaces
This is athlete’s foot’s territory: It thrives in shared communal areas like locker rooms and showers, where the floors might never get a chance to fully dry off. The wet and often humid air in a steamy locker room is heaven for fungal growth. If these areas aren’t sanitized enough, it’s likely that bare feet can pick up fungal spores. Obviously, this is why it’s called athlete’s foot.
Wearing shower shoes or sandals in these spaces is the best way to avoid fungal or even possible bacterial infection. This is where $5 flip-flops come in handy. When showering, it’s also good to use soaps that are targeted towards preventing fungal infection so that any excess amounts of yeast on the skin are washed away.
Certain Medications
The skin’s surface has a healthy balance of bacteria and fungi to maintain proper appearance. If bacteria becomes too abundant, it can lead to acne breakouts. If fungi becomes too abundant, it can lead to fungal infections.
Certain medications, like antibiotics, might increase the risk of fungal overgrowth on the skin. Antibiotics decrease bacteria in the body; if that bacteria was keeping the fungus in balance, and now it’s gone, the fungus may grow (there are other factors at play too, this is pretty generally speaking). So these medications might kill both the bad and good bacteria in and on the body. Without the competition, fungi can thrive on the skin.
Antibiotic medications have been found to cause fungal infections, especially after prolonged use.5 Talk to your doctor about ways to treat a fungal infection when you’re also taking antibiotics, corticosteroids, immunosuppressants, or other medications that might make the body susceptible to fungal growth.
Weakened Immune System
The body’s immune system is its first defense against fungal infection, or any infection for that matter (bacteria, viruses). If the immune system is weaker than usual, for a variety of reasons, it might be easier for a fungal infection to take off. The immune system is boosted by a nutritious diet, regular exercise, stress management, and sleep, so a lack of those can weaken it. Certain diseases, like diabetes, lupus, HIV, and AIDS, can deplete the immune system. Cancer patients taking chemotherapy, smokers, and people with a history of alcoholism also have weakened immune systems; according to the CDC, these people are at a higher risk for fungal infection, as if having cancer wasn’t enough to worry about.6 But a weakened immune system isn’t usually the root cause of a fungal infection.
Stress
Stress can increase your risk for fungal infection, but there are usually other, more significant factors at play (like a damp environment on the skin). Excessive stress and anxiety can weaken the immune system, which lowers the body’s defense against skin threats like an overgrowth of fungi.7
Managing stress is important for general physical and mental health, so if you’re having trouble managing stress, talk to your doctor or therapist about what you can do—but fungal infections happen regardless. That’s why antifungal creams exist.
How do you treat a fungal infection?
Treating fungal infections normally begins with a topical antifungal cream or prescribed antifungal medications, either topical or oral (or a combination). However, fungal infection treatments depend on the exact type of infection you have, and how severe it is. Some can clear up in two weeks, others may take longer.
“Treatments are aimed at either decreasing the amount of yeast on the skin with antifungal agents, topically or orally, like ketoconazole or Diflucan,” explains Dr. Caren Campbell. “Or you can calm down the allergic response that’s happening [on the skin] with an anti-inflammatory cream that’s either a steroid, like hydrocortisone, or a steroid-free anti-inflammatory cream, like Elidel or Tacrolimus.”
Talk to your doctor or dermatologist to chart the best course of action for your infection.
Treating Athlete’s Foot
Athlete’s foot, also known as tinea pedis, is one of the most common fungal infections out there. It affects the skin on the feet, but it can also appear on the hands and nails. The itchy, peeling, sometimes blistering rash is particularly common among athletes or people who share communal surfaces, like locker room showers and floors. The fungus lives on those damp surfaces and transfers to the feet and in between the toes.
Treating athlete’s foot typically begins with over-the-counter antifungal topical creams or ointments specifically marketed for athlete’s foot. These can be rubbed directly onto the affected area. Antifungal sprays and soaps can also be incorporated into shower routines to stop, or prevent, athlete’s foot from spreading.
The first step in preventing athlete’s foot is to wear shower shoes in public or shared areas, and making sure to wash and fully dry feet before putting on socks and shoes.
Treating Tinea Versicolor
Another common fungal infection is tinea versicolor. It’s a fungal infection that affects the pigmentation of the skin, hence the word “versicolor.” Someone with tinea versicolor might have patches appear that are lighter or darker than the surrounding skin. What’s happening is that the yeast that normally lives on the skin changes form, sinks beneath the surface level of the skin, and creates azelaic acid.
“Azelaic acid interferes with pigment production,” explains Dr. Caren Campbell. “So it causes these little white patches on the skin. And especially if you tan the skin, those areas won’t tan.”
Studies have found that tinea versicolor is more common in tropical climates, where the humidity and heat can spark fungal growth. These patches might itch, but they usually don’t feel like anything. Hormonal changes, oily skin, or hot and humid weather are frequent triggers of a tinea versicolor flare-up.
Like most fungal infections, you can try alleviating the symptoms of tinea versicolor with over-the-counter antifungal topicals and ointments, as well as dandruff shampoos used as body washes. But if those don’t work, a doctor can prescribe an oral medication.
Treating Jock Itch
Jock itch, or tinea cruris, presents itself in areas in and around the groin. Similar to athlete’s foot, it’s named because it is most common in people who exercise frequently and work up a serious sweat. The sweaty skin, combined with clothes that might not be letting air flow in, become a perfect environment for fungus to grow. Jock itch is an itchy, warm rash that’s uncomfortable and unsightly, though it’s not usually serious.
Jock itch can be treated with appropriate antifungal topicals and creams usually explicitly labeled with something like “jock itch relief.” If the skin is having an itchy, inflamed reaction, a doctor might recommend a steroid cream.
“When [yeast is] overgrowing in the groin, sometimes we do use steroids,”—like hydrocortisone— says Dr. Caren Campbell. “But if you put a steroid on it long-term, it can create a good environment for the fungus to overgrow again, and so then the fungus drives down into the hair follicle, which makes the infection worse.”
In some cases, a doctor may prescribe a stronger medication to treat jock itch, but be sure to use the medicine as recommended. Just because the visible rash is gone doesn’t mean that the fungus itself has been eradicated.
Fungal Infections and Light Therapy
A newer possible treatment for fungal infections is light therapy.7 This is a prescribed targeted light that blasts concentrated artificial UV rays on affected areas of the skin without risking skin cancer. Some studies have found this method has had some success in alleviating various fungal conditions, though it’s still being studied and depends on the type of fungus at the root of the problem.8 Light therapy is more common as a treatment for other skin conditions, like [psoriasis.]
However, Dr. Caren Campbell says, “I do not ever prescribe light therapy for fungal infections. Topical and oral antifungal treatments are best. Getting light on fungal infections, like tinea versicolor, makes the color change in the affected skin stand out more from the unaffected skin.”
How do you prevent a fungal infection?
Fungi thrive in warm, dark, and moist environments. Keeping this in mind can be key for preventing infection in the future.
Wear Loose, Breathable Clothing
Tight-fitting clothes can play a role in breeding fungal growth. This is because moisture becomes locked between the fabric and the skin. Without proper airflow and circulation, moisture can cause excess fungus to grow on the skin.
Dr. Joyce Imahiyerobo-Ip a board-certified dermatologist and the CEO of Vibrant Dermatology in Greater Boston, MA, points to clothing as a factor that contributes to pityrosporum folliculitis, often called fungal acne. “It can occur when you wear tight occlusive clothing or fail to shower right after an intense workout.” Usually it isn’t just the clothing that’s causing the infection, but perhaps sitting in the sweaty clothes for too long after you’ve exercised.
(If you’re thinking, but my workout clothes say “sweat-wicking”—yes, that’s true, they do wick sweat away from the body, to an extent. If you realize your workout clothes, and your skin, are damp from sweat, consider that a warning from the microscopic fungus on your skin. So get out of those clothes.)
Wearing looser clothes, whether during exercise or everyday, can generally help allow the body’s surface to cool off, helping to keep the skin’s natural fungus levels in a healthy place. This is especially important before and during exercise, but it’s true for anyone prone to sweating, anyone who lives in a warm climate, or who works outdoors.
Have a Good Shower Routine
By far the best way to prevent fungal infection is to continually practice positive hygienic habits. This includes showering regularly, changing clothes often, and cleaning shared surfaces in the home, like the bathtub and bathroom floor.
For fungal infections like athlete’s foot, jock itch, and fungal acne, it’s important to shower as soon as possible following a sweaty workout. This will wash off fungus-causing sweat as well as excess fungus on the skin. If you’ve had a fungal infection in the past, you can prevent future infection by washing with soaps that are specifically labeled antifungal, like dandruff shampoos.
As important as showering is drying off afterwards, notes Dr. Caren Campbell. For male patients who might be prone to fungal infections in the groin area, like jock itch, she instructs: “When they get out of the shower, have them blow-dry the area, making sure it’s super dry.”
If showering at the gym itself is the only option, be sure to wear shower shoes to prevent catching a fungus from unclean floors and surfaces.
Also, regular hand-washing helps prevent spreading fungal infection if you have one yourself. (So wash your hands after applying an antifungal cream to an infected area.)
Avoid Sharing Personal Equipment
Because fungal infections are contagious through direct contact, it’s important to avoid sharing clothing and towels that might pass along the fungus. This is also why your gym has all those signs about wiping down equipment after use.
Fungal infections spread through contact, not the air. So people with fungal infections don’t need to be quarantined from society. To prevent spreading it to others, keep your hands washed, surfaces cleaned, and keep the infected area from contacting others.
Citations
1 Spectrum of Mycoses by Thomas J. Walsh and Dennis M. Dixon. Medical Microbiology.
2The skin microbiome by Elizabeth A. Grice and Julia A. Segre. Nat Rev Microbiol.
3Seborrheic Dermatitis and Dandruff: A Comprehensive Review by Luis J. Borda and Tongyu C. Wikramanayake. J Clin Investig Dermatol.
4Treating Onychomycosis by Phillip Rodgers, M.D. and Mary Bassler, M.D. Am Fam Physician.
5Role of Antibiotics and Fungal Microbiota in Driving Pulmonary Allergic Responses by Mairi C. Noverr et al. Infect Immun.
6Stress Weakens the Immune System by American Psychological Association.
7,8Antimicrobial photodynamic therapy: an effective alternative approach to control fungal infections by Ludmila M. Baltazar et al. Front Microbiol.
Additional References:
Acne Vulgaris: Treatment Guidelines from the AAD by American Family Physician.
Get Updates
There’s more to come.
Sign up to receive periodical updates on Mass Index, and to be the first to know when Soft Services launches new products. (If we don’t have any updates, we won’t email you.)























